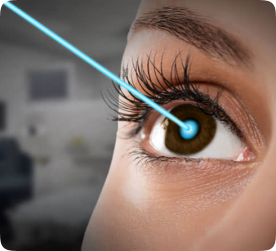
I'm glad to share my happiness, I had my PRK LASIK SURGERY, CONTOURA VISION Surgery went well and very much satisfied, definitely will suggest to friends and family
Our Services
Discover our comprehensive range of eye care services to ensure a brighter
tomorrow for you or your family.
Doctors At Win Vision
18+ experienced eye specialists out of 6 Centers across Telangana and Andhra Pradesh.
Trusted by thousands
Join the thousands of satisfied patients who trust Win Vision for their eye
health and vision care needs.
I am very much happy with the service and Win Vision is one of the best hospital i have seen and maintain neatness and public relations. Very much happy to recommend to others also.
Excellent service and hospitality. Both my parents got operated here for cataract. My father admire s the way dr. Srilakshmi receives patients.
I had great experience visiting the win vision. beerappa help me alot in navigating the service and provided best experience in time service. Last 5 years I visiting the win vision, I always had a great service by staff, doctors and other at Kukatpally and Gachibowli branch
Excellent service, explained in detail with regards to patient on going treatment and usage of medicines Dr pragathi mam was kind towards patience, understands the patient througly and advises back as per patient need. Thanks to win vision moosarambagh branch for all ur on-going support at need
We came hear for cataract surgery it was very Smooth experience happy with service Dr Jyotsna Madam is very excellent doctor.gave proper advice she is very down to earth... My overalla experience is good.. highly recommend hospital...
The Hospital is very clean and neat setup.Ideally located. Was able to take my Father 87 yrs for a checkup. The staff were courteous and efficient. The Doctor after examination explained everything to the patient with utter patience. Advice checkup after 6months.No unnecessary medicine or surgical intervention for cataract developing. Overall the experience was very good.
I was really pleased with my overall experience at the eye hospital, I was immediately put at ease by the staff's extreme friendliness and professionalism. The facility had the newest machinery and technology available. The doctors addressed all of my questions, took the time to thoroughly explain everything, and demonstrated a high level of expertise. There was an extraordinary amount of care and attention to detail. I heartily urge anyone looking for excellent eye care to check out this institution!
We visited win vision eye hospital Kukatpally branch for cataract surgery for my wife Bala Surya kumari.starting from the reception and optom check up..everything went in a smooth manner..and doctor gave good explanation for our problem and surgery process was excellent..and counsellor also explained everything..my overall experience in win vision hospital is awesome.. definitely highly recommend hospital in Kukatpally...
Video Testimonials
Watch our video testimonials to hear directly from our patients about the
exceptional care and guidance.
Awards & Recognitions
15 Years of Excellence Awarded and Recognised by Leading Health Organisations.
Mission + Values
Expanding Win Vision to cover Hyderabad, Secunderabad, Vijayawada, Telangana, and Andhra Pradesh, with plans for 100 medical and optical outlets in rural areas to improve healthcare access and quality.
Our Mission
Our Values
Begumpet
6-3-868, 2, Greenlands Rd, Greenlands, Begumpet, 500016.
Moosarambag
16-11-741/5, Indira Nagar, Moosarambagh, Hyderabad, 500036
Gachibowli
1-73/JH/4 & 11,Sy no.:50 Challa's, beside Chandana Brothers, 500032
Kukatpally
2-22-298/8/2/A BESIDE, Kalamandir Rd, Housing Board Colony, 500072.
A. S. Rao Nagar
1-18-8/6, beside chennai shopping mall, Swamik Nagar, 500062
Vijayawada
RS.No.10/8, D.No.59-12-11, Ward No.8, Polyclinic Rd, beside Hotel Mayur Inn, Gayatri Nagar Urban, Vijayawada, AP-520008