News
Blog
KERATOCONUS
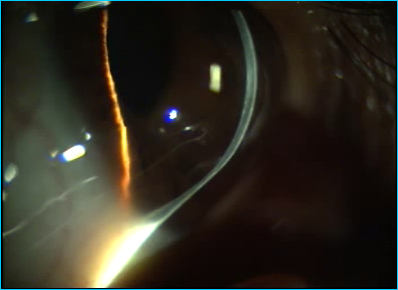
Keratoconus is a corneal thinning disorder in which the inferior paracentral Cornea thins and protrudes forwards. (Figure 1)Though Keratoconus commonly involves inferior paracentral Cornea, cases of superior Keratoconus are also available in literature. The reported incidence of Keratoconus is 1:1000 to 1:20000.Keratoconus seems to be commoner in Asians where it is of early onset and severe. The onset is usually during the second decade. The disease affects the quality of vision and hence causes reduced quality of life.
PRESENTING SYMPTOMS
Blurred vision and frequent changes of spectacle power are the common presenting symptoms.
EYE RUBBING
In addition to heredity, there seems to an association of eye rubbing and development of Keratoconus. It looks like eye rubbing is also involved with progression of Keratoconus and development of acute corneal hydrops.
Various reasons for eye rubbing in Keratoconus patients are as follows
1) Some patients of Keratoconus say they rub their eyes as they felt it would improve their vision
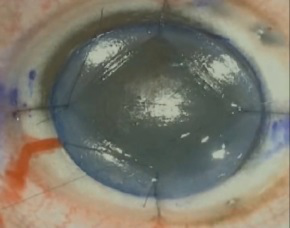
2) Patients of vernal keratoconjunctivitis and severe ocular allergy rub their eyes vigorously and later develop Keratoconus. (Figure 2 ) In patients with severe ocular allergy, topographic indices are found to be abnormal.Any patient with myopic astigmatism should be followed up carefully for the development of Keratoconus if they have severe allergy.
3) Lid margin disease – patient rub their eye because of irritation and itching
4) Patients with Leber’s Congenital Amaurosis develop Keratoconus as these patients rub their eyes to stimulate their retina
5) Down’s Syndrome patients rub their eyes as they are mentally retarded.
6) Oculodigital reflex. We have seen a child with acute corneal hydrops in left eye, right eye being absolutely normal. History revealed, child had habit of sucking the left thumb and whenever she sucks her thumb, she keeping on pressing the left eye with index finger.
Clinical features:
Any myopic astigmatism which is increasing or vision not improving to 6/6 or 20/20 should be suspected to have Keratoconus.
SIGNS
- REFRACTION-
- Myopic astigmatism
- Scissors reflex because of areas of myopic and hyperopic refraction.
Slit lamp features showing the clinical findings on slit lamp examination drawings
- Thinning of inferior paracentral Cornea
- Protrusion or ectasia of inferior Cornea
- The area of thinned ectatic Cornea is in the form of cone. Cones in Keratoconus can be round/nipple shaped, oval/sagging and global if the entire cornea is involved. In oval or a sagging kind of cone, a large area of ectatic thin cornea touching the limbus may be seen. In global type, the entire Cornea is conical.
- Vogt’s stria-these are stria or folds just in front of Descemet’s membrane. They disappear on pressure over the eye
- Apical sub-epithelial and Descemet’s level scarring
- Increased visibility of endothelial reflex
- Prominent Corneal nerves.
- Fleischer's ring is deposit of iron in the base of the cone. Fleischer's ring is important for corneal surgeons as entire thinned Cornea needs to be excised during surgery. If residual thinned Cornea is left, then significant astigmatism may remain following surgery requiring glasses or contact lens after surgery.
- Munson's sign – On looking down, the cone divides the lower lid margin. (Figure 3 )
- Rizzuti sign – When a torch light is thrown from the temporal side, in a normal cornea the nasal and the temporal cornea is equally illuminated. In a conical Cornea, the light focused by the cone is seen as a vertical line on the nasal iris.
- Keratometry – Steep Cornea. Any Keratometry reading of more than 47 diopters should be carefully looked at. In Keratoconus, the keratometer mires are malformed and in severe cases, may not be opposed
- Topography - Any patient with topographic evidence of Keratoconus with no clinical features is labelled as forme fruste Keratoconus. Any island of steepening of inferior Cornea should be suspected to have early or forme fruste Keratoconus. Any patient with central cornea of more than 47D, difference in central cornea between the two eyes of more than 1D and difference between inferior and superior Cornea at equidistant points of more than 1D should be suspected of Keratoconus. Various indices including the Rabinowitz Index and Klyce Maeda Index are available to detect forme fruste Keratoconus.
In addition to steep Cornea in Keratoconus, asymmetrical bow tie pattern of astigmatism with skewed radial axis are important topographic features of Keratoconus.
Ocular and systemic associations of Keratoconus:
Though there a number of associations reported following are seen in practice more often
- Retinitis pigmentosa
- Leber's optic atrophy
- Ocular allergy including vernal Keratoconjunctivitis
Systemic associations:
- Marfan’s Syndrome
- Ehler Danlos Syndrome
MANAGEMENT
General measures. Avoid eye rubbing, do frequent washing of eyes, in allergy cases. Cold compression is suggested for relief of symptoms
The main goal of treatment of keratoconus has changed over the last few years from that focused mainly on improvement of visual acuity to an array of newer modalities focused on the prevention of progression of the disease.
- Spectacles. Reduced visual acuity due to keratoconus is initially managed with spectacles. When spectacles fail to adequately correct visual acuity, contact lenses are the next option.
- Contact lenses. Contact lenses often provide better vision than spectacles by masking irregular astigmatism (higher-order aberrations). For mild or moderate irregularities-soft, soft toric or custom soft toric-contact lenses can be used. Severe irregularities require rigid gas permeable (RGP) lenses in order to mask the irregular astigmatism. Various specialized RGP lenses, such as Super Cone, and Rose K, have been developed for keratoconus. Another alternative is the piggyback contact lens, where a soft lens is fitted to the cornea and an RGP lens is placed on top. For highly irregular corneas, gas-permeable scleral contact lenses are the last option.
- Intrastromal corneal ring segments ( INTACS ): Contact lens-intolerant patients with clear central corneas may benefit from intracorneal ring segment insertion.
- Phakic intraocular lenses ( ICL). Surgical techniques other than laser corneal refractive procedures should be considered for the correction of residual refractive error in the post-ICRS keratoconus patients. One alternative is the use of anterior or posterior phakic IOLs, including toric lenses, either alone or after implantation of ICRS.
- Cornea Collagen Cross linking ( C3R): The disadvantage of the previously mentioned procedures is that none adequately prevent keratoconus progression that occurs due to the underlying biomechanical corneal changes.
- Keratoplasty: In advanced cases of keratoconus where all the above mentioned modalities of treatment are not helpful, transplantation of the cornea needs to be done. The conical shaped cornea ( 8-8.5mm central part ) is replaced by a healthy donor tissue. Newer techniques of transplantation have come in vogue where only anterior layer or the front part of the cornea is damaged there by improving the longevity of the donor cornea in these patients ( DALK).
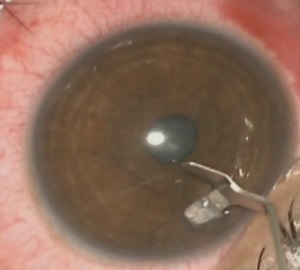
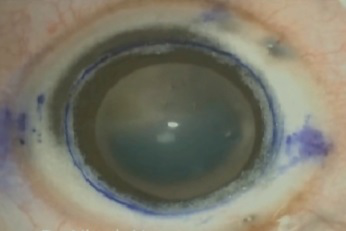
Figure 1. Keratconus with ectasia of Cornea and apical scarring

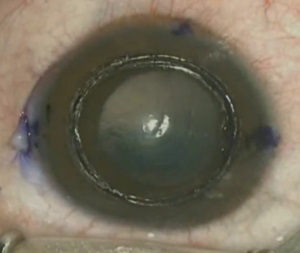
Figure 2. A case of severe allergy which can predispose to Keratoconus
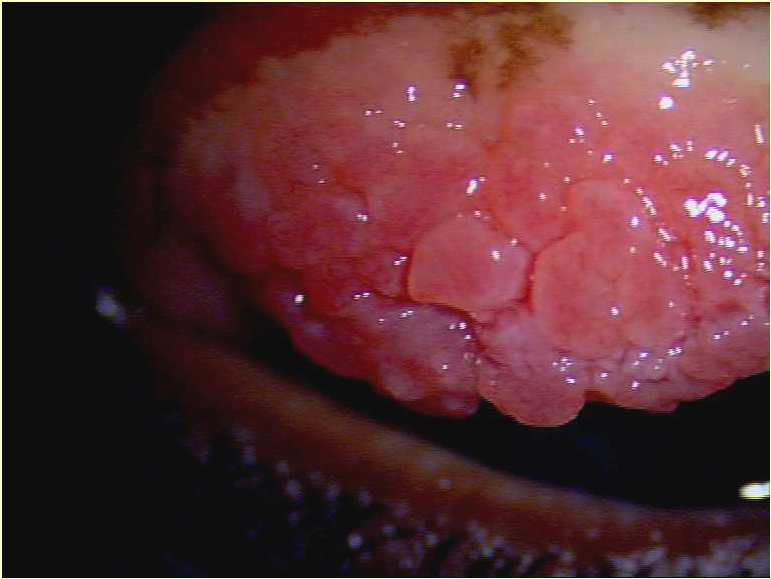
Figure 3. A case of Keratoconus showing Munson’s sign
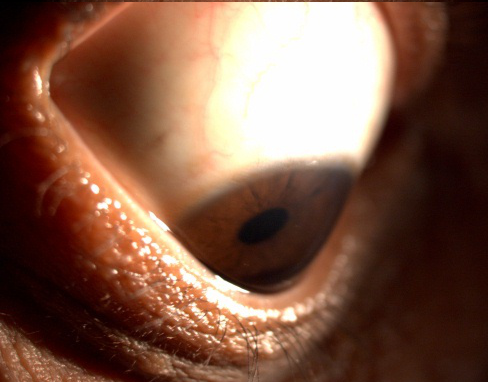
Figure 4 Steps of Intracorneal rings (INTACS) surgery
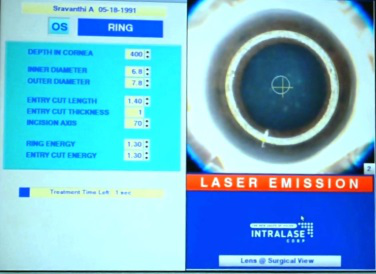


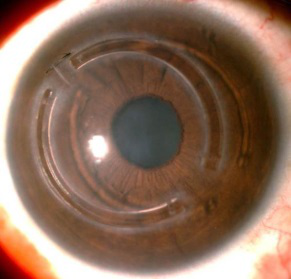
a-intrastromal channels being prepared with femtosecond laser at 70% depth.
b- Channels being opened by Y spatula.
c- superior/larger intac being inserted.
d- inferior/smaller intac being inserted.
e- Final outcome with intacs being symmetrically placed.
Figure 5 - Steps of DALK surgery

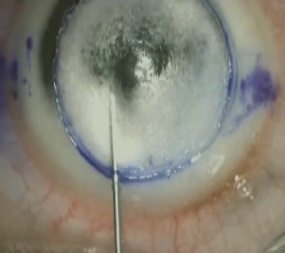

a - Advanced Keratoconus
b - Partial trephination
c - Anterior stroma being removed which would facilitate in the deeper injection of air for the big bubble
d - Big bubble being achieved with bent 26G needle
e - Bare DM after removal of the stroma
f - DM being stripped from the donor cornea
g - Donor sutured on the recipient bed with intermittent 10-0 nylon sutures
Figure 7.The clinical picture following DALK surgery for resolved hydrops
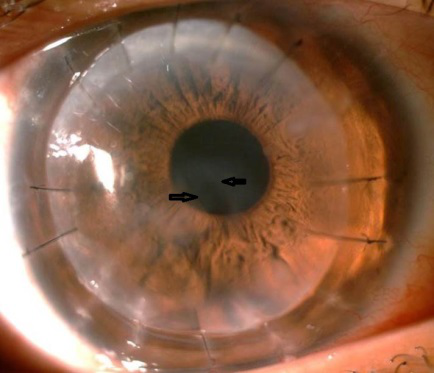
Figure 8.The clinical picture of PMCD. Note the inferior band of thinning with ectasia of normal Corna above the thinned area